Brain Tumors & Cancers
A tumor is an abnormal mass of cells, sometimes benign or malignant. Benign tumors are non-cancerous and typically don’t spread, or metastasize, to other parts of the body. Malignant tumors are cancerous and have potential to spread through the body. Primary brain tumours are those that started in the brain itself. Most malignant brain tumors are secondary cancers seeded from cancer in another part of the body.
Malignant tumors grow at different speeds depending on a number of factors and are classified as Grade 1, 2, 3 or 4. Grade 4 tumors are also known as high-grade brain tumors and the rest are referred to as low grade tumors.
Symptoms
Often times brain tumors grow slowly without causing any symptoms for many weeks as your brain adapts to the new tissue. Sometimes, tumors are discovered incidentally while undergoing diagnostic tests for unrelated conditions. Brain tumors can have nonspecific symptoms, making them more difficult to distinguish from other conditions.
Blurred vision, double vision or loss of vision.
Recurring and frequent headaches.
Seizures.
Loss of balance not caused by peripheral neuropathy or benign vertigo.
Weakness on one side of the body.
Changes in mood and personality not caused by medications.
Cognitive impairment unrelated to dementia.
Speech issues.
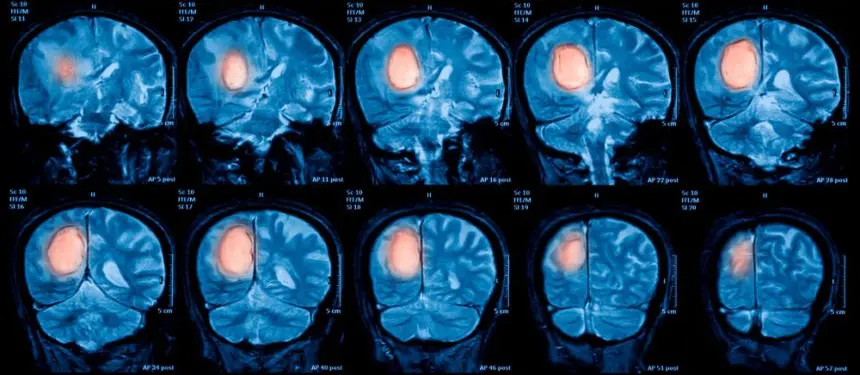
Diagnosis
If you are experiencing any of the above symptoms, contact your physician to assess your overall health and a physical examination. Initial examination by a physician can screen for abnormalities in your cognition, sensations, motor strength, reflexes, coordination and balance. Based on your symptoms and examination, imaging such as CT, MRI (Perfusion or Functional), PET and MRS may be required. At times, a tissue biopsy may also be pursued.
Although, blood tests alone are not used to diagnose brain or spinal cord tumors, other types of cancers can be detected by finding tumor markers - which are substances made by cancer cells or your body’s normal cells in response to cancer. These markers are specific to the type of cancer. For example, Calcitonin for thyroid cancer, PSA for prostate cancer, AFP for liver cancer etc. Though there are no specific markers for brain or spinal tumors, the amount of cell-free DNA (cfDNA) in the bloodstream is known to be an indicator of glioblastoma (GBM) - a type of deadly brain tumor.
Treatment
Each of the 100-150 different types of tumors and cancers requires a different treatment approach. Many times, a combination of more than one type of treatment is required. Surgery, Radiation therapy, Stereotactic radiosurgery, and Chemotherapy are currently available mainstream treatment options in addition to medicines that inhibit cancer growth such as tyrosine kinase inhibitors, proteasomes inhibitors, mTOR inhibitors, PI3K inhibitors, histone deacetylase inhibitors, hedgehog pathway blockers, BRAF inhibitors etc. All cancer growth blockers can cause side effects. If you are experiencing any serious side effects of your medications, please contact your medical provider.
The 5 year survival rate for those who receive brain cancer diagnosis is less than 33% according to National Cancer Institute of UK. However, advancements in early diagnosis and innovative technologies, such as image guided surgery and targeted cancer drugs (MABs, anti-angiogenics, PARP inhibitors etc.) are improving survival rates and quality of life, helping patients live longer, meaningful lives.
What is Image Guided Surgery?
Newer surgical techniques use image guidance technologies known as stereotaxy, surgical navigation, computer assisted surgery, navigated surgery or stereotactic navigation.
Similar to how GPS in a car helps you drive with ease, image guided surgery (IGS) helps navigate a surgeon's precise movements using cameras and electromagnetic fields. IGS helps the surgeon perform safer and minimally invasive procedures to remove brain tumors that were once considered inoperable due to their size and/or location.
Dr. Samadani is an expert in Image Guided Surgery. Please contact Dr. Samadani's office for evaluation.
Make an AppointmentComplex Regional Pain Syndrome
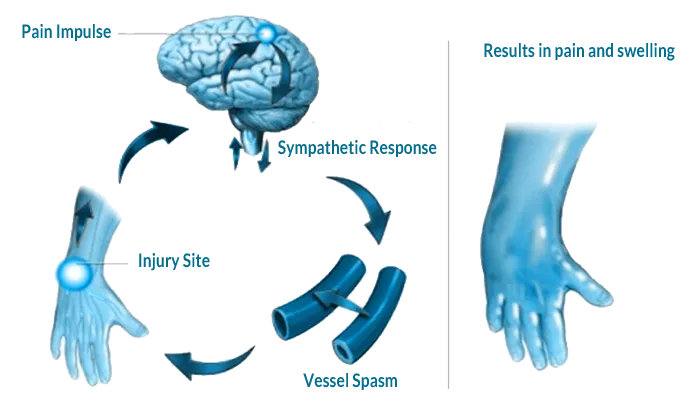
Complex Regional Pain Syndrome (CPRS) is a chronic neurological disorder characterized by disabling pain, swelling, vasomotor instability, sudomotor abnormality, and impairment of motor function. Complex Regional Pain Syndrome (CPRS) generally affects legs and arms. CRPS develops after an injury, a surgery, a stroke or a heart attack. The pain is prolonged and far more intense than that of the initial injury. CRPS is also known as Reflex Sympathetic Dystrophy (RSD or CRPS-Type I) and Causalgia (CRPS-Type II).
Majority of CRPS conditions are the result of improper function of the peripheral C-fiber nerve fibers that carry pain messages to the brain. Their excessive firing triggers inflammation that leads to burning sensation, swelling and pain.
Symptoms
Symptoms change over time and vary from person to person. Patients who suffer CRPS may exhibit the following symptoms:
Unprovoked or spontaneous pain
Excessive or prolonged pain
Changes in skin temperature, texture, color, and/or swelling
Abnormal sweating
Abnormal nail and hair growth
Stiffness in affected joints
Excessive bone growth
Impaired muscle strength and movement
Sensitivity to touch or cold
Continuous burning or throbbing pain
Muscular atrophy, spasms and tremors
Diagnosis
Most often CRPS is triggered by nerve trauma or injury to the affected limb that damages the thinnest sensory and autonomic nerve fibers. Fractures, surgery, sprains/strains, burns or cuts, poor circulation etc. are some of the common reasons why people develop CRPS. CRPS develops only in the limbs because circulation is constrained there.
Currently, no single, specific test can identify CRPS. Diagnosis includes a detailed examination by a neurologist, nerve conduction studies, imaging nerves by ultrasound or magnetic resonance imaging (MRI) and triple-phase bone scans.
Treatment
Oftentimes, most mild cases recover on their own. General treatment options include the following.
Rehabilitation and physical therapy is the single most important treatment for CRPS. Patients who develop post-traumatic stress disorder can benefit from psychotherapy. Graded motor imagery and pain medications also help. Spinal cord stimulation or other types of neural stimulation (peripheral nerve stimulation and motor cortex stimulation) via implantation of a neuro-stimulator device is an effective option for some. Transcranial Magnetic Stimulation (rTMS) and stimulation at the peroneal nerve at the knee has proven effective in some cases.
Implantation of spinal-fluid drug pumps to deliver pain-relieving medications directly into the fluid can be an option in severe cases. Some patients can benefit from medical marijuana, behavior modification, acupuncture, relaxation techniques and other similar alternative therapies. In certain clinical settings, intravenously given ketamine has been shown to be useful in treating pain that does not respond well to other treatments.
Sympathetic nerve block, surgical sympathectomy, severing injured nerves or nerve roots and amputating the painful limb are a few rare treatments that are not as frequently used as other remedies.
Dr. Samadani is a world renowned expert on nerve and spinal injuries. Consult Dr. Samadani for thorough evaluation and seek eraly treatment.
Make an AppointmentSpinal Tumors
Spinal tumors can develop around the spinal column, within the spinal cord or around the nerves. Tumors can occur on multiple places in or around spine. Just like any other tumor, these can be benign (i.e. non-cancerous) or malignant (i.e. cancerous). Sometimes, the tumors originate within the spine (primary tumors) or spread to spine due to some other form of cancer (secondary tumor). Majority, up to 70%, of malignant spine tumors are secondary tumors.
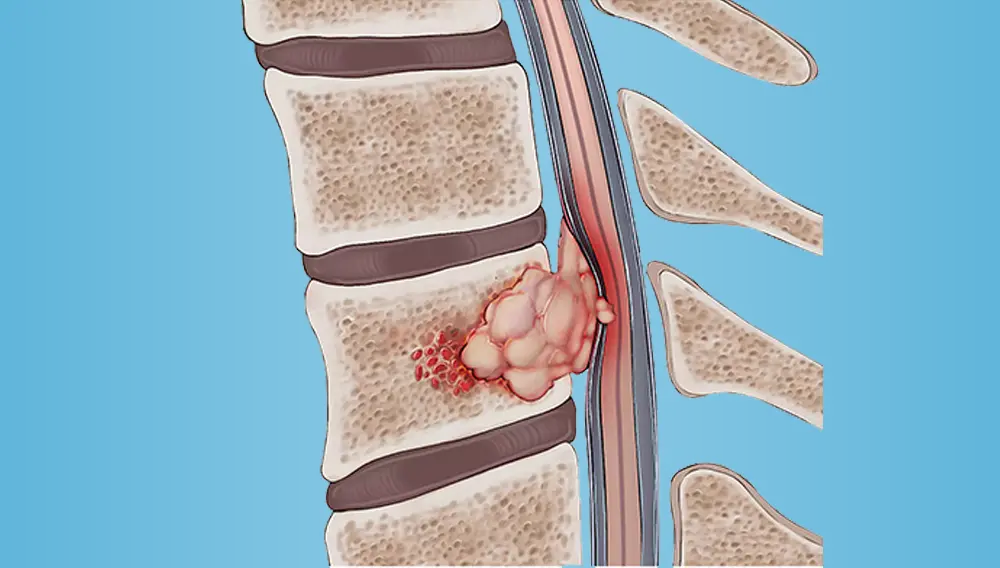
Spinal tumors are categorized based on their locaton – cervical, thoracic, lumbar, intradural, extradural, intramedullary or extramedullary. Extradural tumors are generally cancerous while others are benign.
Symptoms
Spinal tumors certainly show discernable symptoms. Each type of tumor presents itself differently. Symptoms include:
Persistent lower/middle back pain
Weakness in arms, chest, and legs
Loss of bladder/bowl control
Difficulty in walking
Numbness and tingling
Spinal deformity
Diagnosis
A thorough physical examination and radiological imaging such as X-Rays, CT scans, MRIs will reveal the presence of spinal tumors. A bone scan using Technectium-99 will be helpful in detecting primary bone tumors, infection and bone abnormalities. Sometimes, a biopsy might also be needed for further analysis of the tumor.
Treatment
Treatment for spinal tumors depends on the stage, location and type of tumor. Generally, an inter-disciplinary team of oncologists, radiologists and spinal surgeons will evaluate and determine the correct course of action.
Some tumors can be effectively treated with radiation and chemo-therapy, especially where surgery is either not possible due to location and size of the tumor or because the tumors are asymptomatic.
Complete en bloc resection could potentially be adequate in some surgical cases. Generally metastatic tumors are good candidates for surgery, especially when they don't respond well to radiation or chemo therapy. Intractable pain, spinal cord compression and fractures are also indications for surgical intervention.
Thoracic and lumbar spinal tumors that affect both posterior and anterior vertebrae pose a special surgical challenge. As is in with any major surgery, spinal tumor surgery presents certain complications and risks which need to be carefully evaluated based on patient's overall health, condition and location of the tumor and the prognosis.
Dr. Samadani is a leader in the treatment of rare and complex spinal tumor cases that require expert skills and groundbreaking technology.
Make an AppointmentSpinal Cord Injury
Damage to the spinal cord or nerves within the spinal canal is considered spinal cord injury. A traumatic spinal cord injury happens due to a sudden blow or cut to the spine as is when a person is an automobile accident. A spinal cord injury causes permanent loss of strength, sensation and function below the site of the injury.
Complete or partial paralysis occurs in the areas of the body that are controlled by the nerves associated with the damaged vertebrae and those below. The higher the injury, the more paralysis there is. For example, damage in the cervical segment can result in paralysis of the chest, arms, and legs (tetraplegia, or quadriplegia). Damage in thoracic, lumbar, or sacral segments can result in paralysis of the legs and lower body (paraplegia). Breathing is affected only by injuries high on the spinal cord. But bowel and bladder control can be affected no matter where the spinal cord is injured.
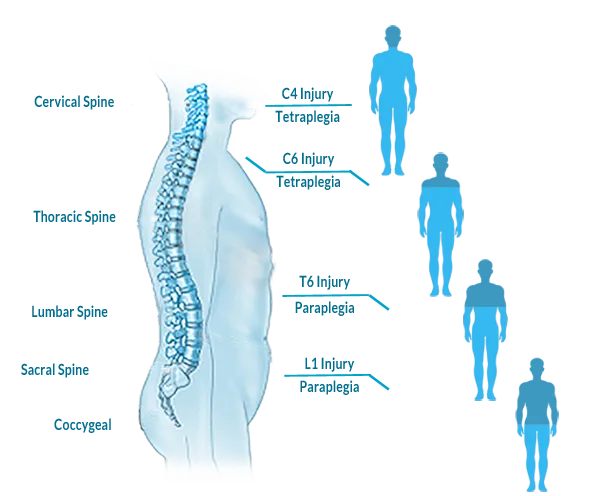
Spinal cord injuries are divided into two types: incomplete and complete. An incomplete spinal cord injury is one in which there is some motor or sensory function below the affected area. A complete spinal cord injury is one in which all ability to control movement (motor function) are lost below the injury. There are three types of complete spinal cord injuries: Tetraplegia, Paraplegia and Triplegia. The most severe type of complete spinal cord injury is Tetraplegia. This causes paralysis and can affect every limb.
There are three common types of incomplete spinal injuries: Anterior Cord Syndrome, Central Cord Syndrome and Brown-Sequard Syndrome. Incomplete spinal cord injuries are more common than complete injuries.
Symptoms
Your neurologist will examine you to determine the neurological level and completeness of your injury. Given below are some of the symptoms:
Loss of movement
Loss of sensation
Loss of bowel or bladder control
Changes in sexual function, sexual sensitivity and fertility
Pain or an intense stinging sensation
Paralysis of limbs
Difficulty breathing, coughing or clearing secretions from your lungs
Uncontrolled muscle spasms
Changes in reflexes
Back pain
Diagnosis
A quick test for sensory function and movement can indicate spinal cord injury. A definitive diagnosis of spinal cord injuries requires a CT scan, MRI or X-ray. These tests help the doctors determine the abnormalities within the spinal cord, injury location, level and completeness.
Treatment
Unfortunately, spinal cord injury cannot be reversed and is permanent. Treatment focuses on preventing further injury and empowering people with a spinal cord injury to return to an active and productive life.
Treatments include medications, immobilization and surgery to remove fragments of bones, foreign objects, herniated disks or fractured vertebrae. Experimental treatments to stop cell death, control inflammation and promote nerve regeneration are being actively researched and being tested but not yet mainstream treatment options.
Research is underway in developing sophisticated, functional electrical stimulation devices, that use electrical stimuli to control arm and leg muscles to allow people with spinal cord injuries to stand, walk, reach and grip.
Please consult Dr. Samadani to find out how she can help you.
Make an AppointmentHydrocephalus
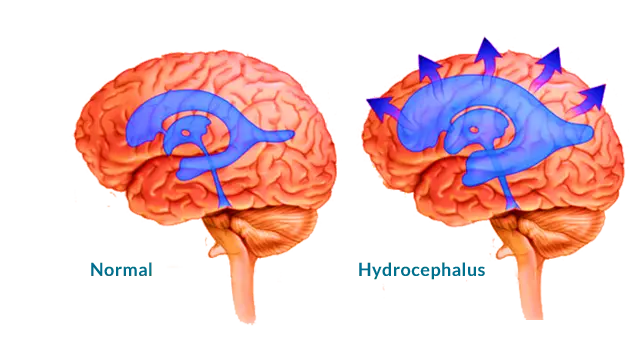
Cerebrospinal fluid (CSF) keeps the brain buoyant allowing the brain to float within the skull. It functions to cushion the brain to prevent injury, remove waste products of metabolism and maintain a constant pressure within the brain.
Abnormal accumulation of cerebrospinal fluid in the brain causes the cavities (ventricles) of the brain to fill & swell casuing a condition known as hydrocephalus. Swelling increases the cerebral pressure that can lead to tissue damage in the brain and loss of function.
Hydrocephalus occurs mostly in infants and older people (over 60 years of age). Some infants are born with the condition and it progresses gradually as they age.
Symptoms
Symptoms vary depending on age. Older people show very different symptoms than infants. Other brain related conditions mimic hydrocephalus and therefore, symptoms must be carefully evaluated by a trained neurologist.
Infants
Abnormally large head that grows in size rapidly
Soft bulge on top of head
Problems sucking and feeding
Sun setting (downward looking) eyes
Occasional seizures
Irritability
Sleepiness
Other symptoms include headache, blurred or double vision, problems with balance, loss of developmental progress like walking or talking, poor appetite and coordination, frequent urination and loss of cognition including memory.
Adults
Loss of bladder control
Declining cognitive skills and memory
Shuffling gait and difficulty walking
Loss of balance and coordination
Slow movements
Difficulty remaining awake or waking up
Diagnosis
A neurological exam and brain imaging is required to diagnose the condition. Neurological exam includes age appropriate evaluation of memory, coordination, movement, muscle strength, reflexes and cognition. Imaging tests may include CT, MRI and Ultrasound. A spinal tap (lumbar puncture), fundoscopic examination and intracranial pressure monitoring (ICP) may also be done.
Treatment
Hydrocephalus is generally treated surgically. Dr. Samadani treats adult onset Hydrocephalus. She performs the following surgical treatments. Parents of infants who are affected by Hydrocephalus may contact a pediatric neurosurgeon.
Shunt
A shunt is a flexible tube inserted into the brain to drain excess fluid into abdomen or chest so it can be absorbed by the body. A shunt does not treat the underlying cause of the condition but certainly provides significant relief.
Endoscopic Third Ventriculostomy (ETV)
A small hole is made at the bottom of the third ventricle to divert CSF and relieve pressure. Sometimes, this is done along with choroid plexus cauterization (burning off some tissue that produces CSF) to reduce CSF production.
Make an AppointmentArteriovenous Malformation
An arteriovenous malformation (AVM) is an abnormal connection between groups of arteries and veins. The capillaries between arteries and veins get unusually tangled forming direct connections and start abnormal blood flow. Such abnormal connectivity disrupts normal blood flow and oxygen circulation leading to hemorrhage, stroke, brain damage and occassionally death. It is currently unknown how and why AVM's form.
When AVM's form, the capillaries disappear, blood does not slow down, doesn't deliver oxygen and nutrients to the tissues and flows too fast directly from an artery to a vein.
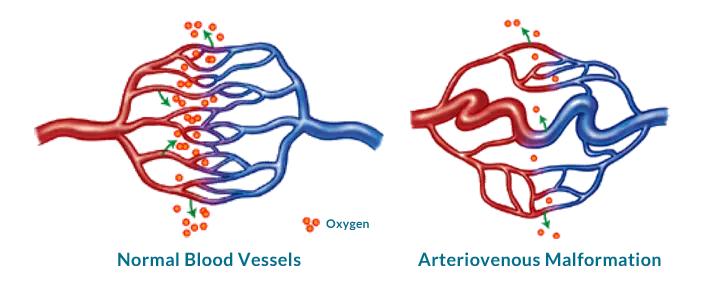
Tissues surrounding AVM don't get enough blood supply leading to tissue damagae that could be permanent. AVM's can occur in any part of the body, including brain. AVM's in the brain or close to the spinal cord, are called neurological AVMs, and are most likely to cause long-term problems. AVM's in brain can be successfully treated, if diagnosed early. The greatest potential danger of AVMs is hemorrhage which remains undetected because it is not significant or large enough.
Symptoms
The symptoms vary depending on where AVM occurs. Most people with AVM's don't show any symptoms and won't experience any problems for long time. AVM's are often discovered when they rupture or cause significant symptoms.
Buzzing in the ear
Blurred vision or double vision
Headache and backache (spinal AVM)
Seizures
Muscle weakness
Facial paralysis, loss of sensation
Changes in smelling, walking and speaking
Dizziness & Loss of consciousness
Diagnosis
History and physical exam are two initial means of diagnosis. Imaging tests such as ultrasound, MRI or CT might be required to make a final determination. Magnetic resonance angiography captures the pattern, speed and distance of blood flow through the vascular abnormalities to aid in final diagnosis. However, cerebral angiography is the gold standard of detecting AVMs and may be required to get better understanding of the structure of the blood vessels.
Treatment
Size, location and stage (pain or loss of function) guide the course of treatment. Currently there are no medicines to treat an AVM, although some medicines are in experimental stage. However, there are medicines to help manage symptoms such as seizures, headaches and back pain.
Endovascular embolization and sclerotherapy are common treatments for AVM that are currently available. Embolization and sclerotherapy can reduce the size and symptoms but are not cures for AVM. Stereotactic radiosurgery is also an option to treat AVMs.
For some AVMs, surgery is an option, especially if there is a high risk of bleeding and if it is in a part of the brain that can be safely operated on.
Make an AppointmentChiari Malformation
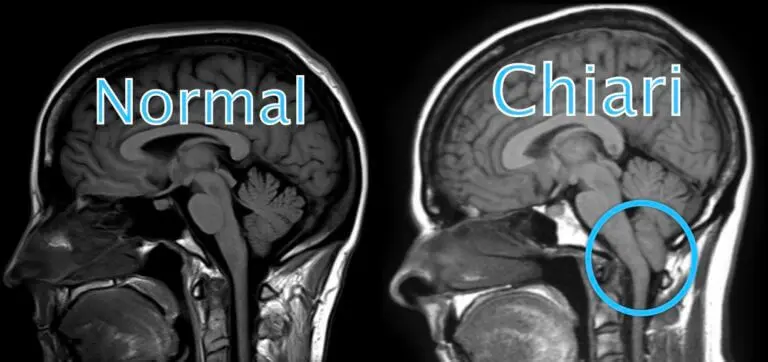
Chiari malformation occurs when part of the brain expands into the spinal canal.Common reason for this condition is misshaped skull or smaller than usual skull which pushes the brain down into the canal.
Depending on the area of the brai that is pushed downward, Chiari is classified into Type 1, Type 2 or Type 3. Generally, Type 2 and Type 3 are congenital (i.e. present at birth) while Type 1 develops as the person grows into adulthood. Type 3 malformation is more problematic than the rest since the cerebellum is pushed through the back of the skull. Hence, it is associated with higher mortality and may cause neurological problems. Chiari can lead to complications such as Hydrocephalus, Spina bifida, Syringomyelia and Tethered Cord syndrome as well.
Symptoms
Chiari doesn't generally cause any serious symptoms and hence is diagnosed during tests that are unrelated to this condition.
Type 1 Chiari can show the following symptoms:
Headache
Dizziness
Neck pain
Gait Issues
Numbness and tingling
Speech Issues
Swallowing difficulty
Poor motor coordination
Type 2 Chiari can show the following symptoms:
Changed breathing pattern
Swallowing issues
Weakened limbs
Changes in eye movements
Diagnosis
Chiari is generally diagnosed using several imaging methods such as MRI, X-Rays (CT) or Ultrasound. All of these are non-invasive, simple, painless procedures.
Treatment
Treatment is dependent on type of Chiari, severity of the condition and perhaps, even age. Asymptomatic patients are monitored long term and no treatment is generally recommended.
However, in severe cases with pronounced symptoms, surgery is generally performed to stop or slow the progression of the condition and relieve the pressure on the brain and spinal canal.
Please contact Dr. Samadani's office for evaluation.
Make an AppointmentSpondylolisthesis & Spondylolysis
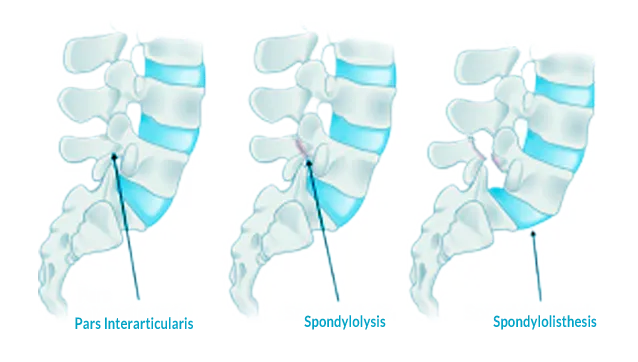
These two are related conditions but not same. Spondylolysis is a stress fracture or crack in spine bones. Most commonly, this fracture occurs in the fifth vertebra of the lumbar spine, although it sometimes occurs in the fourth lumbar vertebra. Fracture can occur on one side or both sides of the bone. Spondylolisthesis is when a vertebra slips out of place, resting on the bone below it. Vertebra may slip out of place due to a degenerative condition. Spondylolysis and spondylolisthesis occur in the lumbar spine. Both cause low back pain.
Spondylolisthesis can be either low grade or high grade, depending upon the amount of slippage. A high-grade slip occurs when more than 50% of the width of the fractured vertebra slips forward on the vertebra below it. Patients with high-grade slips are more likely to experience significant pain and nerve injury needing surgery to relieve their symptoms and prevent further deterioration.
Types of Spondylolisthesis
Congenital SpondylolisthesisCongenital spondylolisthesis occurs when a baby’s spine doesn’t form the way it should before birth. The misaligned vertebrae put the person at risk for slippage later in life.
Isthmic SpondylolisthesisIsthmic spondylolisthesis happens as a result of spondylolysis. The crack or fracture weakens the bone.
Degenerative SpondylolisthesisAging causes the disks that cushion the vertebrae lose water over time. As the disks thin, they are more likely to slip out of place.
Pathogenic SpondylolisthesisDue to bone disease such as metastatic disease, tumor, osteoporosis.
Traumatic spondylolisthesisCaused because of a fracture of the neural arch
Post-surgical spondylolisthesisA vertebra slips out of place after spinal surgery.
Symptoms
Lower back pain is the most common symptom of spondylolysis. It usually gets worse during exercise or other physical activity, especially when someone leans back a lot. Spondylolysis also can cause buttock and leg pain, and tight hamstrings. The pain may extend to the buttocks and down the thighs.
The following are other symptoms:
Muscle spasms in the hamstring.
Back stiffness.
Difficulty walking or standing for long periods.
Pain when bending over.
Numbness, weakness or tingling in the foot.
Headache.
Diagnosis
Evaluation of this condition includes a review of the medical history and a physical exam followed by several imaging methods such as MRI, X-Rays (CT) or Ultrasound. A bone scan can be used for early detection of a stress fracture of the pars.
Sophisticated imaging techniques such as single-photon emission computed tomography (SPECT) bone scans and magnetic resonance imaging (MRI) scans of the spine can help in evaluating the physiological changes associated with spondylolysis and help distinguish between active and inactive spondylolysis.
Treatment
The grade is based on how severe the spondylolisthesis is. Low-grade (I or II) is less serious and usually doesn’t need surgery. High-grade (III and IV) is more serious. You may need surgery, especially if you’re in a lot of pain.
Spondylolisthesis is treated with the strengthening of supportive abdominal and back muscles through physical therapy. Other treatments include:
Rest
Anti-inflammatory medicines
Steroid shots
Physical therapy and
Bracing
If you continue to have severe pain and disability after physical therapy, surgery may be an option.
Untreated and severe spondylolisthesis may lead to a condition called cauda equina syndrome. This is a serious condition where nerve roots in the lower back called the cauda equina are compressed leading to loss of feeling in the legs and also can affect the bladder and cause paralysis.
Please contact Dr. Samadani's office for evaluation.
Make an Appointment